Can exercise and probiotics boost the effectiveness of flu vaccines?
The very last thing we should do is to blame people for their suffering which covid-19 has caused to innocent people across the World. Many fit men and women have been struck down, for no fault of their own, but the reality is that people with lifestyle associated medical conditions do have an increased odds of developing serious consequence of this virus – read more
Lifestyle factors many not just be relevant to catching covid or suffering more serious consequences of an infection, they may have an influence on the effectiveness of the vaccine – if studies published related to the Flu vaccine are found to apply to the covid vaccine. Many scientist feel they would as the fundamental modes of action are the same although this is yet to be confirmed. The two factors which have potential benefits are exercise and taking a course of probiotic supplements:
Exercise and vaccines

Being physically activity has been found to improve immunity in general but a commentary published in this month’s Human Vaccines and Immunotherapeutics the author, Dr Kate Edwards advises that a bout of exercise can bring about profound changes in the immune system, such as increasing circulating cell numbers. She cites a study conducted by scientists at the Iowa State University in the USA that showed mice who ran leisurely for about half an hour after vaccination showed maximum resistance to any side effects of the flu shot. .read study
In humans, two further new studies, involving runners, swimmers, wrestlers, cyclists and other athletes, suggest that training amplifies the vaccine response, a finding with particular relevance now, as the Covid-19 vaccine programme is being rolled out. It is already known that people who work out often tend to catch fewer colds and other viruses than sedentary people but now these studies suggest that if you exercise in the hours before a flu shot, you likely will develop a stronger antibody response than if you rest.
The first study from Saarland University in German was published in January in Brain, Behavior, and Immunity, compared 45 athletes with 25 young people who were healthy but not athletes to serve as a control group. They found the athletes showed a “more pronounced immune response,” with presumably better protection against flu infection. The second study, which was published in July in Medicine & Science in Sports & Exercise, tried to find out when it was best to exercise and found it did not matter if it was before or after a jab – the benefit was the same
Although these studies are not conclusive, exercise is a very healthy activity so Dr Edwards and other scientists believe it would be advisable to increase levels around the time of your vaccine and afterwards. It should be noted, however, that our bodies react in different ways and advises people not to overdo physical activity after a vaccination but engage in moderate activities such as cycling, or resistance exercise and avoid dehydration by drinking plenty of fluids.
Probiotic supplements and vaccines

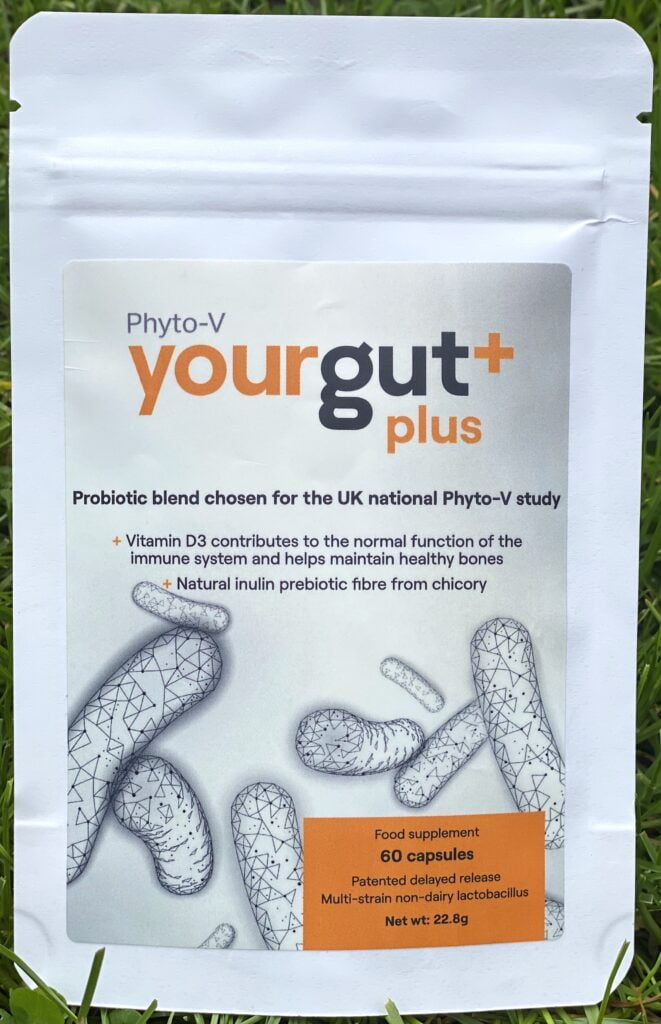
As regards boosting the effectiveness of a vaccinations, a recent systematic review and meta-analysis evaluated twelve scientifically robust randomised studies involving a total of 688 participants. They scrutinised the influence of prebiotics /probiotics/synbiotics supplementation on vaccine responses to influenza vaccination. Dr Yeh and his colleagues reported that patients taking mainly lactobacillus probiotics with prebiotics in supplements form were found to have higher influenza hemagglutination inhibition antibody titers after vaccination in all A/H1N1, A/H3N2, and B strains (20%, 19.5%, and 13.6% increases, respectively). They concluded that concomitant prebiotics or probiotics supplementation with influenza vaccination may hold great promise for improving vaccine efficacy. They did comment that further studies are warranted and of course the role specifically for covid-19 has yet to be determined.
In the mean time, healthy measures to improve gut health seem very sensible and that could include a good quality lactobacillus supplement.
Vitamin D and the Covid vaccination

Furthermore, emerging data suggests that better vitamin D repletion and correcting deficiency can reduce covid-19 severity and mortality, information that has led to correction of vitamin D deficiency being included in protocols for treating Covid-19 patients [Kory]. A recent report using UK Biobank data found a strong inverse association of serum 25(OH)D values, prospectively, with Covid-19 severity, abolished by adjustment for obesity and ethnicity which both reduce serum 25(OH)D concentrations directly by well-understood mechanisms, meaning that mechanistically predictable protective effects of adequate vitamin D repletion were not excluded. [Hastie, Boucher]
We don’t know, for sure that adopting lifestyle measures to increase vitamin D including taking an extra vitamin D supplement can help the effectiveness of the covid-19 vaccination but it’s benefit for the flu jab do suggest it could be a simple, safe and cheap adjuvant to the vaccine especially in high risk groups for Covid-19 which are well-known to coincide with groups at high risk of vitamin D deficiency.
 References
References
Lee MD, et al. Does Vitamin D Deficiency Affect the Immunogenic Responses to Influenza Vaccination? A Systematic Review and Meta-Analysis. Nutrients. 2018 Mar 26;10(4):409. doi: 10.3390/nu10040409. PMID: 29587438;
Sutherland JP, Zhou A, Leach MJ, Hyppönen E. Differences and determinants of vitamin D deficiency among UK biobank participants: A cross-ethnic and socioeconomic study. Clin Nutr. 2020 Nov 25:S0261-5614(20)30639-7. doi: 10.1016/j.clnu.2020.11.019. Epub ahead of print.
Kaufman HW, et al. SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels. PLoS One. 2020 Sep 17;15(9):e0239252. doi: 10.1371/journal.pone.0239252. PMID
Kory P, Meduri GU, Inglesias J, Varon J, Marik P. Clinical and Scientific rationale for . the “MATH+” hospital treatment protocol for COVID-19. (Analytic Rev.) J Int Care Med. 2020;1-20. DOI: 10.1177/0885066620973585
Hastie CE, et al. Vitamin D concentrations and COVID-19 infection in UK Biobank. Diabetes Metab Syndr. 2020 Jul-Aug;14(4):561-565. doi: 10.1016/j.dsx.2020.04.050. Epub 2020 May 7. Erratum in: Diabetes Metab Syndr. 2020 Sep – Oct;14(5):1315-1316. PMID: 32413819; PMCID.8.
Boucher BJ. Vitamin D status as a predictor of Covid-19 risk in Black, Asian and other ethnic minority groups in the UK. Diabetes Metab Res Rev. 2020 Nov;36(8):e3375. doi: 10.1002/dmrr.3375. Epub 2020 Jul 31. PMID: 32588937.
.Schuler PB et al. The effect of physical activity and fitness on specific antibody production in college students. J Sports Med Phys Fitness. 1999;39:233–9.[PubMed] [Google Scholar].