What is Cancer?
.
Normal cells grow to their desired size, space themselves out evenly and stick to their original site. They obey instructions from the regulatory systems of the body via hormones and chemicals, and do not divide or replicate unnecessarily and, when they do, do so at a controlled pace. They die when they are supposed to in order to make room for healthy young cells to take over their function.
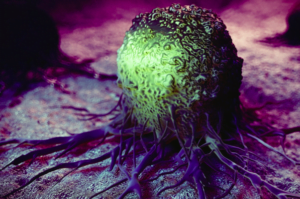
Cancer cells grow as fast as they can, don’t die when they ought to, clamber on top of each other and quickly run out of space in the organ of origin. They not only expand the organ but also infiltrate and invade their neighbouring structures, causing considerable damage. This invasion is one of the hallmarks of cancer. The other way cancers can make room for themselves is to lose their stickiness to the organ of origin and break off and spread (metastasis) to another part of the body and start growing there.
Types of cancers
- Adenocarcinomas – glands in breast, pancreas, prostate, gut and lungs
- Squamous cell – surfaces of skin, lungs, oesophagus, head and neck
- Urothelial cancers – linings of blabber or tubes within the kidney
- Sarcomas – from muscles, nerves or connective tissues
- Lymphomas – starting in lymph nodes
- Leukaemia’s – starting in blood or bone marrow
- Gliomas – from cells which support the brain
Even though cancers have some common characteristics, their growth rate, pattern of spread and response to different treatments can vary considerably, making it vital to know exactly what type you and your doctors are dealing with. Even cancers of the same type can behave very differently depending on the genes and receptors which are activated, and pathologists now spend a great deal of time profiling cancers into subtypes in order to guide oncologists on developing individualised treatments.
The management of individual cancer types for different patients is very complex, and the emphasis of one treatment over another can vary depending on which organ the cancer originates in and which cells it is derived from. The management of patients with the same cancer can vary enormously depending on the grade of the cancer (how aggressive the cells look down a microscope) and its stage (how far it has spread). Even the treatment of individuals with the same stage and grade can change depending on the condition and general health of the patient.
How do cancer cells survive and thrive?
- Grow faster (proliferate)
- Not die when they reach the end of their life cycle (apoptosis)
- Recruit blood vessels to feed themselves (angiogenesis)
- Lose their stickiness to the site of origin (loss of adhesion)
- Grow into adjacent organs (invasion)
- Spread through the body (metastasise)
- Thrive in adverse environments
The biochemical mechanisms which cancers have adopted in order to survive and spread are outlined below, an understanding of which is imperative when attempting to understand cancer and devise effective treatments.
1. Rapid proliferation
Generate their own growth signals – Normal cells require growth signals before they can move from a dormant state into an active proliferative state and cannot grow without these signals. Cancer cells, on the other hand, grow and proliferate on their own because they have learnt to generate their own growth signals – growth signal autonomy.
Overriding anti-growth signals – Normal cells stop growing when they need to in response to checkpoint signals which tell them to switch off. Cancer cells have learnt to be insensitive to antigrowth signals, allowing them to continue to grow despite overcrowding themselves and their neighbours.
Loss of hormonal control – Via a process called de-differentiation, cancer cells, although starting off similar to cells in the organ of origin, quickly evolve into more aggressive forms. These undifferentiated cells lose the receptors (antennae) which pick up signals from hormones, allowing them to grow unchecked and become resistant to hormonal therapies.
Loss of circadian rhythm – Normal cells slow down at night, helping them repair spontaneous or acquired genetic damage and preserve energy. Some cancers have learnt to switch off the normal circadian biochemical clock, allowing them to grow 24/7.
2. Immortality
The ability of tumour cell populations to expand in number is determined not only by the rate of cell proliferation but also by the rate of cell attrition. In stark contrast to normal cells, which only divide a finite number of times before they enter into a permanent state of growth, arrest or death, cancer cells divide and proliferate forever, or at least until the host dies or treatments and lifestyle measures stop them. There are a number of explanations for this immortality, but the three most well known are:
Damage to the DNA policeman – A widely known protein which protects DNA is P53 – nicknamed the ‘DNA policeman’. If a cell is partially damaged, P53 slows the cell cycle and allows DNA repair to take place. If repair is not possible, it does not allow the cell to divide with damaged DNA. Instead, it triggers pathways to tell the cell to commit suicide – apoptosis. Some people are born with a defect in this policeman gene (known as Li-Fraumeni syndrome). As you can imagine, they usually develop multiple cancers at a very early age in life. Acquired defects in P53 have been identified in over 50% of cancers. These defects allow cells to pass through the various stages of the cell cycle rapidly – too fast for apoptosis pathways to be triggered – allowing cells to continue growing and dividing albeit with partially defective DNA, leading to mutations and eventually cancer.
Resistance to programmed cell death (apoptosis) – Independent of P53, cancer cells can develop changes in their apoptosis mechanisms. In this case, even if P53 is able to send a signal to the cell telling it to commit suicide, the suicide apparatus is not functional, and the cell carries on growing and dividing.
Telomere protection – The immortality of malignant cells can also be explained by their ability to maintain the length of a small strip of nuclear proteins at the end of each strand of DNA – the telomeres. Like slow-burning fuses, telomeres become shorter each time a cell divides, acting as a kind of cellular clock ticking down a cell’s age. Eventually, they are depleted, and the cell enters a permanently arrested state called senescence. To escape this inevitable demise, about 90 % of human tumours are able to boost intracellular levels of an enzyme called telomerase, which adds nuclear proteins to telomeres, thus turning the clock backwards.
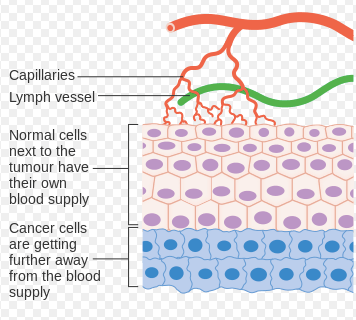
3. Recruitment of more blood vessels (angiogenesis)
4. Loss of adhesion, invasion and metastasis
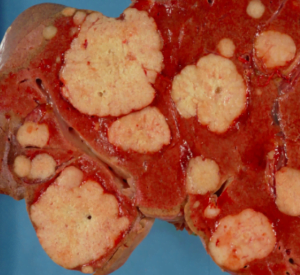
By dividing faster and not dying when they should, cancer cells soon run out of space. In order for them to survive, they invade adjacent organs and metastasise to other parts of the body. The first stage of expansion involves losing the glue that keeps a normal cell in place – loss of adhesion. The molecules responsible for this glue are called cell adhesion molecules (CAMs) and include cadherins, integrins and selectins. In normal tissues, they are responsible for wound healing and tissue repair. Once cancer cells have blocked their production, they are free to migrate. Migration occurs when cells release chemicals which break down the extracellular matrix proteins and fibroblasts – barriers to their spread. They can either spread directly into tissues or migrate along nerves and lymphatic/blood vessels. Sometimes they migrate, initially, just within the gland of origin, such as the breast ductal system. In this case, they are called carcinoma in situ. However, if they have managed breach the basement membrane of the organs or glands, they are called invasive cancers and have the capacity to spread to distant sites in the body via the bloodstream – metastasis.
Metastasis requires a sequential series of complex biochemical steps before triggering significant lesions which inevitably lead to the demise of the host. Recent evidence suggests that the first stages of metastasis can be an early event and that 60% of patients have initiated the metastatic process by the time of diagnosis. Even patients that display no evidence of tumour dissemination are still at risk of metastatic disease. Approximately one-third of women, for example, who are sentinel lymph node-negative at the time of surgical resection of the primary breast tumour will subsequently develop clinically detectable secondary tumours.
5. Thriving in adverse environments
Rapid turnover of cancer cells with damaged DNA and impaired repair processes makes them more susceptible to damage from reactive oxygen species (ROS) which could potentially kill them. ROS can be generated from continued carcinogen exposure or formed naturally as a byproduct of oxidative phosphorylation. Cancer cells have developed a number of adaptations in order to counteract ROS, including developing resistance to oxidative damage by decoding oxidative-stress signals and converting them into pro-survival signals which actually promote growth, even in highly oxidative environments.
Cancers have lower oxygenated environments, which are inevitable in rapidly growing masses that have a tendency to outstrip their blood supply, even with enhanced angiogenic capacities. To cope with this, cancer cells prioritise glycolysis which can function anaerobically.
The rapid proliferation also creates a much higher demand for nucleic acids and amino acids such as glutamine. In both normal and cancer cells, a small percent of those proteins do not fold properly during the synthesis process. When that happens, the cell activates its unfolded protein response (UPR), which slows down the making of new proteins while the misfolded proteins are refolded. Eventually, the buildup of misfolded proteins becomes toxic and leads to cell death. Cancer cells form a lot of misfolded proteins, but they have learned to use the UPR to slow protein synthesis when needed and efficiently handle the backlog of mis-folded proteins. This helps them survive in conditions that would kill normal cells.